By Michael Burger, EHR and EDI Practice Lead
We’ve seen a flurry of regulatory activity lately from the Centers for Medicare and Medicaid Services (CMS). Among all the requirements, three related to electronic prescribing (ePrescribing) may have escaped the attention of electronic health record (EHR) vendors. They are: the hard cutover to NCPDP SCRIPT 2017071 in 2020 and the adoption of two new ePrescribing functionalities related to opioid prescribing, which will be required of hospitals. Vendors should act now to ensure readiness in time for January 2020.
Migration to the new version of SCRIPT. CMS just announced the adoption of NCPDP SCRIPT 2017071 in a final rule (discussion begins on page 16636). Primarily, this is the periodic ePrescribing standards update for Medicare Part D. But, there’s an important twist. The new rule retires NCPDP SCRIPT 10.6 as the Part D ePrescribing standard and requires use of the newer NCPDP SCRIPT 2017071 beginning on January 1, 2020. In the past, CMS-mandated standards changes included a transition phase during which both the new and old standards were allowed. This was discussed extensively in the CY 2013 Medicare Physician Fee Schedule Final Rule.
Not this time. Because version 2017071 is NOT “backward compatible” with version 10.6, everyone will have to cut over in a year and a half--and all at the same time. If past is prologue, there will be a last minute scramble for system upgrades to ensure compliance. We have heard that some vendors are lobbying for the implementation date to be extended. In fact, CMS already pushed back the cutover by a year. Even if the implementation is postponed further, it only delays the inevitable challenge of a simultaneous cutover. The hard cutover on January 1, 2020, has the makings of a redux of the transition to X12 5010 back in January 2012, with everyone stampeding to get ready in a short time. Heads up, EHR vendors.
New ePrescribing functionalities. There also are big changes coming to the EHR Incentive Programs (aka Meaningful Use), which were renamed Promoting Interoperability Programs in yet another final rule. Now, CMS will be requiring use of two new measures related to ePrescribing of opioids by hospitals and critical access hospitals. The Query of PDMP (Prescription Drug Monitoring Programs) measure will be optional in calendar year (CY) 2019 and will be required beginning in CY 2020. The Verify Opioid Treatment Agreement measure will be optional for both CYs 2019 and 2020. The new measures must be incorporated into certified EHR technology (CERHT). EHR vendors should be planning now to incorporate these new requirements (and certification) for their CEHRT-compliant products.
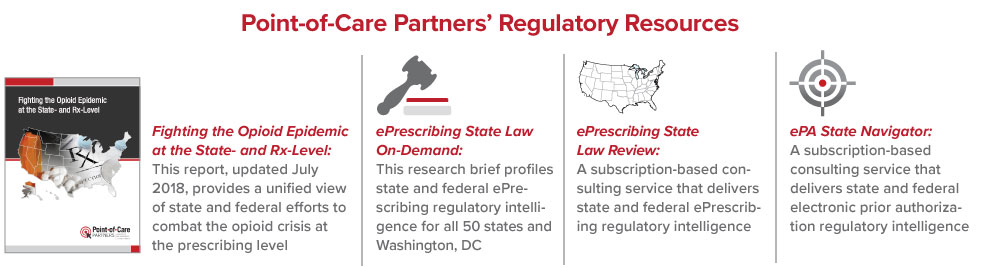
Do you have questions about these sweeping changes or other ePrescribing and EHR issues? Reach out to me at michael.burger@pocp.com. Want to keep current with ePrescribing laws and regulations? Feel free to drop our regulatory specialists a line at regulatory@pocp.com.