This website uses cookies so that we can provide you with the best user experience possible. Cookie information is stored in your browser and performs functions such as recognising you when you return to our website and helping our team to understand which sections of the website you find most interesting and useful.
HIT Perspectives: New Model Can Help Payers Realize Return on Investment From Electronic Prior Authorization
HIT Perspectives – June 2017
New Model Can Help Payers Realize Return on Investment From Electronic Prior Authorization


By Pooja Babbrah and Jocelyn Keegan, Senior Consultants
Payers increasingly are looking for ways to optimize their processes and return on investment (ROI). Electronic prior authorization (ePA) represents such an opportunity yet despite its promise, the transaction is, unfortunately, underutilized among many payers. A new ePA maturity model developed by Point-of-Care Partners (POCP) can help payers and pharmacy benefit managers (PBMs) identify their progress with ePA adoption as well as steps they can take to move forward with ePA to optimize their ROI.
Why ePA? An increasing number of medications require preapproval — or prior authorization (PA) — from payers before they can be dispensed. This traditionally has been a cumbersome, time-consuming and frustrating manual administrative process. The reason: PA is based on numerous phone calls and faxes — plus the exchange of lots of paper — among physicians, pharmacies and payers. Recognizing that there has to be a better way, stakeholders from across the industry – led by POCP’s Tony Schueth — developed an electronic prior authorization (ePA) standard using the National Council for Prescription Drug Programs (NCPDP) standard for electronic prescriptions (SCRIPT). The ongoing goal is to incorporate the standard into the electronic health record (EHR) work flows of physicians, pharmacies and payers. A draft standard was piloted in 2011, and the standard became a reality a couple of years later. As the standard has matured over the years, EHRs and payers have become increasingly able to handle ePA transactions.
The business case for ePA is pretty clear. There are significant administrative costs associated with manual PA processing, which can be mitigated by computerized processing. According to a recent article in Health Affairs, physicians spend the better part of $37 billion annually ($83,000 per doctor) thrashing out PA and formulary issues with payers. According to another estimate, doctors spend 868.4 million hours on PA each year — not counting time devoted by other staff members.
ePA reduces the time spent on each PA by all participants. According to a survey by the American Medical Association, most physicians experience a delay in excess of a week for their PA request to be processed. PA also is a work-flow drag on pharmacies. In contrast, prospective ePA — which allows advance approval of an ePA request — often can be processed within minutes when payers are equipped to electronically accept and process PA requests, as well as return real-time responses using the NCPDP standard.
Perhaps most importantly, the difficulties inherent in trying to obtain a PA significantly affect patient care and safety. Nearly 40% of PA requests (roughly 75 million) annually are abandoned due to complex procedures and policies and the hassle factor. Moreover, nearly 70% of patients encountering paper-based PA requests do not receive the medication originally prescribed.
Barriers to ePA adoption. It is clear that investing in prior authorization automation is the right thing to do. However, not all ePA is equal. Today, anything “electronic” related to PA may be inaccurately considered ePA. Despite the availability and adoption of the NCPDP ePA standard, the current process remains largely reactive, with providers and pharmacies chasing failed electronic prescriptions because they need a PA.
There are a number of reasons why PA remains a challenge for payers to move forward with prospective ePA. Each payer has evolved its use of ePA through a myriad of business and technology drivers, lines of business and customer-specific constraints. There are also varying state and local regulatory requirements. States continue to enact requirements for ePA for pharmacy and medical benefits, but the rulings vary by state and often do not mandate use of ePA based on the NCPDP standard. In addition, payers struggle with integrating ePA into internal systems — whether they are installed as software or home-grown utilization management systems. Potential inaccuracies of some data concerning PA in electronic prescribing work flows — such as the need for PA for a particular patient —are often confusing or inconclusive for prescribers. Finally, users continue to grapple with EHR design challenges, which both delay and suppress physicians’ adoption of prescriber-driven ePA.
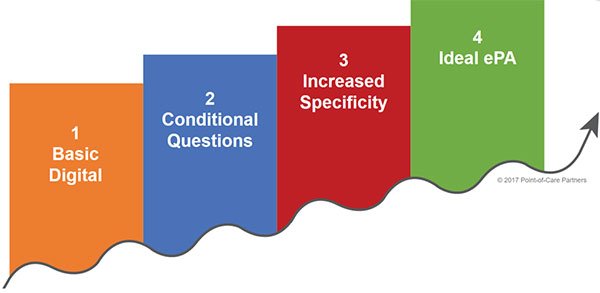
The ePA maturity model. Based on interviews with PBMs, POCP developed an ePA maturity model. With it, payers and PBMs can understand where they are across four levels of maturity (as shown below) and learn more about proven best practices to improve the ROI on their ePA investment. One payer saw a 28% improvement in automation by reengineering supporting processes.
The model is customizable, incorporates NCPDP standards and is designed so users can identify and address gaps that are preventing PA from moving toward a totally electronic process.
Using the ePA maturity model allows payers and PBMs to:
- Create a framework to categorize improvement opportunities. This provides a tool to visualize opportunities across business or client-selected categories. It also allows PBMs to identify patterns for programmatic investment and opportunities. This, in turn, allows them to acknowledge and understand areas of the business so as to avoid or apply only proven best practices. The framework can help identify lines of business that are ripe for experimentation.
- Honestly assess adoption of ePA. Implementation varies among EHRs and providers. Even though the ultimate goal is full automation of the ePA process, outcomes may be improved at every step of the PA process. In fact, any incremental improvement to improve true ePA adoption results in real savings and operational efficiency.
- Determine where organizational adoption lies on the ePA maturity curve. The maturity curve has four inflection points ranging from basic digital ePA to use of conditional questions, to use of more specific questions, and finally to ideal and fully automated ePA using the NCPDP standard. This will allow payers to see at a glance where their organization lies in terms of real ePA adoption and where forward progress can be made.
- Develop and deliver organization-specific recommendations using proven best practices. Using data gleaned from steps 1-3, the organization can assess its status and what must be done to move forward. The goal is to move all process and question sets as far up the maturity curve as possible. For example, the ePA maturity model can help PBMs identify potential lines of business that are ready for process improvement, discuss top strategic goals for PA and explore partnerships or pilots.
Benefits of the ePA maturity model. There are many benefits related to use of the ePA maturity model. Its use will empower a payer to focus on critical technical and process improvements that will increase ROI from ePA. For example, it allows payers and PBMS to:
- Reduce administrative costs and turnaround times.
- Develop a programmatic approach to improve ePA across all functions within their organization.
- Create a common model for ePA to share across the organization to support PA improvements.
Mature organizations will be prepared to handle and create value from the richer patient data set and coded data criteria from a patient’s record to make a more accurate ePA determination.
To be sure, there is much more detail surrounding each section of POCP’s ePA maturity model. POCP can provide a consistent, outside-in assessment on how to move an organization and its partners forward with investments at the points of highest potential return. Let us know how we can put the ePA maturity model to work for you.



