HIT Perspectives – February 2020
FAST: The Coalition Aiming to Strengthen the FHIR Interoperability Infrastructure

By Dana Marcelonis, Account Director, Payer Services

By Dana Marcelonis, Account Director, Payer Services
Health Level 7’s (HL7) FHIR (Fast Healthcare Interoperability Resources) standard is rapidly becoming the standard of choice to enable the exchange of clinical and, increasingly, coverage-related data. Its uptake will continue to accelerate because of work on functional use cases developed by various coalitions, including the HL7 DaVinci Project and the CARIN Alliance.
But the road from inspiration to implementation is not smooth. As coalitions pursue their respective functional use cases, they’re encountering similar challenges stemming from the existing hybrid environment. Just a few examples include how to locate and interact with the right payer without managing scores of one-on-one connections, how to mediate the range of versions and profiles in use, and how to integrate new FHIR exchanges with existing partners and infrastructure.
 It became clear to early adopters that such challenges are common and needn’t be addressed over and over again within and across the individual functional use cases. Enter FHIR at Scale Taskforce (FAST), whose mission is to address those shared architectural barriers and gaps. FAST — convened at the request of industry leaders by the Office of the National Coordinator for Healthcare Information Technology (ONC) — is set to tackle key areas of common challenges and develop forward-looking potential solutions. The aim of these analyses is to address current barriers and establish an interoperability architecture to support FHIR adoption at scale.
It became clear to early adopters that such challenges are common and needn’t be addressed over and over again within and across the individual functional use cases. Enter FHIR at Scale Taskforce (FAST), whose mission is to address those shared architectural barriers and gaps. FAST — convened at the request of industry leaders by the Office of the National Coordinator for Healthcare Information Technology (ONC) — is set to tackle key areas of common challenges and develop forward-looking potential solutions. The aim of these analyses is to address current barriers and establish an interoperability architecture to support FHIR adoption at scale.
Addressing technical challenges.
FAST is taking a Tiger Team approach to address these technical challenges that currently limit FHIR adoption. The first step in addressing these challenges was for the Ecosystem Tiger Team to analyze several functional use cases and identify common barriers. Although the analyses are focused on FHIR, they highlight common infrastructure issues that must be resolved to facilitate interoperability across various standards, technical platforms and use cases.
See the diagram below for brief problem statement descriptions for the FAST Tiger Teams and current proposed solutions still under development.
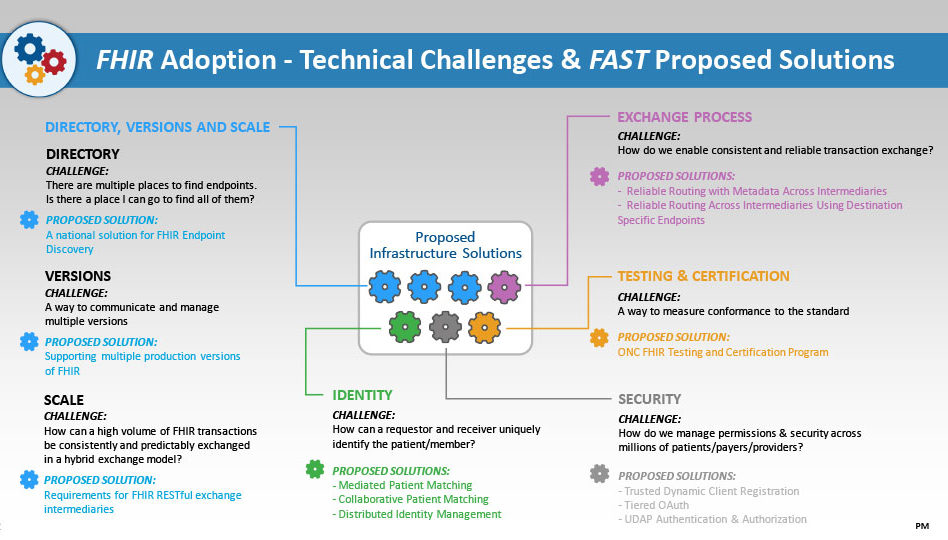
Importantly, these Tiger Teams aren’t working in a vacuum. Each of these proposed solutions has been presented to the FAST Technical Learning Community (TLC) to gain feedback and will be further vetted through smaller sessions with subject-matter experts for refinement and strengthening before they move to the next stage. Artifacts could come in the form of implementation guides, industry guidance or best practices.
Want to get involved?
Request to join a Tiger Team or participate in the TLC. You can sign up to join the FAST Technical Learning Community to get updates, provide input on technical and regulatory barriers, new use cases and potential solutions on the FAST confluence page. There also is a LinkedIn Group. •
Point-of-Care Partners (POCP) can also be a valuable resource on FHIR, program management of multistakeholder initiatives and related matters. We are the project management organization for Da Vinci and provide support staff for FAST (learn more on the FAST Confluence page). We are involved in several stakeholder efforts aimed at health IT standards and adoption. We’d be pleased to explain how these developments affect health IT in general and your organization. If you have any questions, contact me at dana.marcelonis@pocp.com.
In this Issue: