HIT Perspectives – April/May 2020
Take Note of the Health IT Opportunities Emerging From the Final Interoperability Rules of ONC and CMS


By Gary Austin, Payer/Provider Interoperability Lead and Ken Kleinberg, Innovative Technologies Lead


By Gary Austin, Payer/Provider Interoperability Lead and Ken Kleinberg, Innovative Technologies Lead
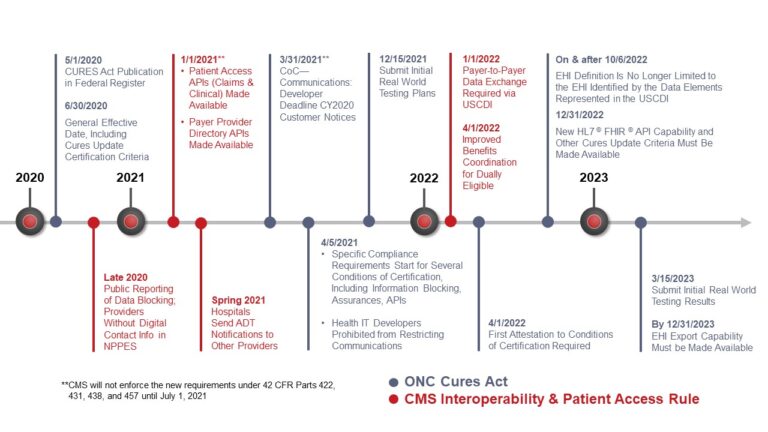
*CMS/ONC Rules Timeline was updated on 11/17/2020 to reflect changes to the deadlines.
The long-awaited interoperability rules from the Office of the National Coordinator for Health Information Technology (ONC) and Centers for Medicare and Medicaid Services (CMS) arrived just as the response to the novel coronavirus disease 2019 (COVID-19) crisis ramped up. As conveyed in our recent blog and March 13 webinar, the rules will be game changers for consumers, payers, providers and technology vendors despite the challenges swirling around the health care system in these uncertain times. Stakeholders should be “heads down” now analyzing how both sets of rules will impact their business.
These rules present opportunities for both operational improvement and market differentiation. It’s critical that your business and development teams understand the value-based care landscape, the impact of other federal rules in play, and how planned releases of named and synergistic standards will be impacted, including how multi-stakeholder groups are using the Fast Healthcare Interoperability Resources (FHIR) today to advance interoperability. Your competitors will be moving full steam ahead on not only meeting rules compliance, but also leveraging the new capabilities for marketplace leadership. Will you be ready? What are some of the opportunities that will arise?
Readiness is one of the most critical issues for all stakeholders. In the past, stakeholders have not always felt urgency around implementation of federal regulations. It’s different with the interoperability rules. Their short implementation timelines—despite the handful of relatively small extensions—coupled with the COVID-19 response will push innovation and adoption forward at rocket speed. As shown in the figure below, time will be of the essence and readiness will be a primary market differentiator.
With short implementation timeframes beginning this fall, stakeholders should ask themselves:
Payer resources. For Payers, it’s critical to identify underlying technology gaps related to patients’ data access, payer-payer data transfer, and creation and maintenance of provider directories. They must understand all the nuances around sharing data singly and in bulk, such as ensuring data accuracy. Payers who do not have the underlying technology in place to accomplish the heavy lift needed for each of these (and most don’t) will need to start building it as soon as possible.
Vendor resources. For health information (health IT) technology vendors, the challenges are somewhat different. They must figure out how to provide patient (and caregiver) access to data across payer and provider platforms. This must be done while conforming to ONC’s certification and information blocking requirements to avoid financial penalties for noncompliance. Are the right technology stacks in place to accommodate APIs? What is on the shelf that will work to fulfill the new mandates? What adaptations will be needed to enable data exchange with older systems that are not FHIR based?
Organizations will have to ramp up quickly to meet the compliance deadlines and avoid penalties. Amid the flurry of preparation, organizations should take the time to identify risks and opportunities. We’ve included some examples, based on Point-of-Care Partner’s long-standing leadership in strategic positioning in the health IT field.
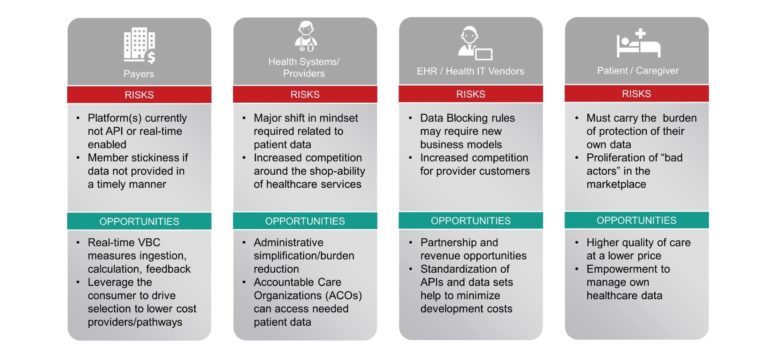
Providers. Providers will also have to make a major mindset shift related to patient data. They sit on a huge repository of data in EHRs and their new required liquidity will necessitate workflow changes. At the same time, increased access to payer data will help improve quality of care. Providers, however, will need to educate patients about how their data might be used by third-party app vendors that operate outside of the Health Insurance Portability and Accountability Act (HIPAA). Protection of data, once it flows to apps, would fall to the Federal Trade Commission, from whom we expect guidance this year.
The new “shopability” of care puts providers in new competitive modes, in which patient recruitment and retention will be influenced by easy access to their data and how they are exchanged. Improved price transparency and lower costs of care could affect reimbursement, which will depend on health IT to provide the necessary data to support payment metrics as well as submit required information. Analytics and artificial intelligence will also have roles in helping make this voluminous amount of data actionable for physicians and operations.
EHR and health IT vendors. These entities will clearly need to make business policy and contract changes and implement new approaches to address data blocking rules. Their provider clients will increasingly be required to share data — vendors who make data sharing “easy” will have a competitive advantage. It will be easier for customers to air usability challenges in the market due to vendors’ inability to fully hide their customers’ complaints behind gag clauses. There will also be increased competition for provider customers, whose business needs also will evolve to respond to the changing regulatory and payment landscapes. The rules are likely to level the playing field among players: big, small, old and new.
Patients/Consumers. The new interoperability rules put consumers, for the first time, firmly in the drivers’ seat for accessing and sharing their own health data. This is primarily done through consumer-facing applications (apps) and health IT tools developed for them from third parties and other stakeholders to access payers and providers via open application programming interfaces (APIs). It will enable consumers to select lower-cost and better performing providers and procedures as well as drive down the costs of care. Additionally, patients will have more data to evaluate their health plan networks and reimbursement/coverage. Low health literacy is still a barrier. Effective patient education programs will be needed to help patients understand their data and how to use them to make informed choices.
These interoperability rules are just one aspect of our nation’s drive to a more consumer-centric health care delivery system that rewards value and which we are all painfully aware now needs to be more agile in responding to health care crises (see our related article in this issue of HIT Perspectives). Another key aspect is advancing the use of standardized health IT transactions that will improve patient access to medications and reduce provider burden. During the past year, we’ve seen a number of related federal rules that will work in concert with these interoperability rules, such as:
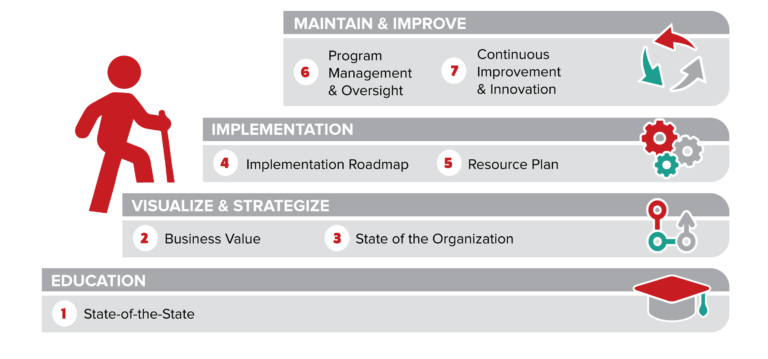
Remember: This is an interoperability journey. It will be vital for stakeholders to design and build supportable strategies, create a roadmap for successful implementation and develop a sustainable organization. POCP is uniquely positioned to guide your organization in the transition to the growing, patient-facing health IT economy. Reach out to us at Gary “Lumpy” Austin (gary.austin@pocp.com) and Ken Kleinberg (ken.kleinberg@pocp.com). We’d love to hear from you.
In this Issue: