HIT Perspectives: 8 Impressions from HIMSS 2019
Previous Article | Next Article
HIT Perspectives – March 2019
8 Impressions from HIMSS 2019

By Tony Schueth, Editor-in-Chief

The book is closed on this year’s annual meeting of the Healthcare and Information Management Systems Society (HIMSS) in Orlando, the go-to meeting for health information technology (health IT). We understand that attendance was down slightly, but there still were more than 40,000 people who spent a lot of time and money to attend, exhibit and make presentations. With its notable focus on real-world efforts to improve the patient journey and noticeable C-suite attendance, the conference lived up to its theme, “Champions of Health Unite.” This makes HIMSS — without a doubt — the best place to catch up on the latest from vendors, clients and various stakeholders. The Point-of-Care Partners (POCP) team used its time productively through face-to-face discussions, attendance at sessions and presentations, discussions with exhibitors and investment of a lot of shoe leather.
There are plenty of reports in the media on various aspects of HIMSS 2019. Instead of a meeting summary, we offer insights on what we learned in Orlando and how they might impact the health IT industry going forward. Here are our top eight takeaways from HIMSS 2019.
- The feds’ regulations drop overshadowed the published agenda. Normally, we provide thoughts on the buzz generated by the keynotes and major announcements at the meeting. This year the buzz was about announcements of new proposed regulations from the Office of the National Coordinator for Health Information Technology (ONC) and the Centers for Medicare and Medicaid Services (CMS). They rolled out unexpectedly at the meeting, grabbing attention away from just about everything else. ONC’s proposed regulation on interoperability and information blocking has been in the works for quite a while. It was long overdue, so we really weren’t surprised when it debuted at HIMSS. Everyone had speculated for months about the details. We heard rumors that some vendors put activities on hold in their app store until the proposed regulation was issued. If that weren’t enough, attendees were really caught off guard by CMS’ long-anticipated proposal that notably would require qualified health plans to give Medicare beneficiaries access to their claims data through FHIR-based open application programming interfaces (APIs). This “proposal” essentially mandates that this must be done by 2020 by all health plans doing business with Medicare and Medicaid and through the federally facilitated exchanges. This “proposal” essentially mandates that this must be done by 2020 by all health plans doing business with Medicare and Medicaid and through the federally facilitated exchanges. The announcements were a major focus. It appeared everyone spent most of their time discussing the proposals and guessing about their contents and impacts, since nobody had the documents in advance or the time to read them at the meeting. The rules drop also overshadowed other big announcements that were made. An example is the Department of Veterans Affairs (VA) joining forces with Apple to make health records available via iPhones to more than 9 million patients in the VA system by this summer. (Click here for our thoughts on the two proposals and their impacts.)
- Accessibility and control of patient data were prominent topics. This continues a theme launched last year by the federal government when Seema Verma, who heads CMS, used her 2018 keynote to announce two initiatives: MyHealthEData and Blue Button 2.0. This year, she introduced the proposed regulation on sharing patient data through APIs, as described above. This continues the administration’s ongoing emphasis on providing data and technology to patients so they can control and direct their own health care. (As an aside, this message, delivered by the keynote panel speakers as what some perceived as a scolding to the electronic health record vendors was received incredulously by the audience of health IT vendors, who were focused more on their provider client base and less on patients.) Also, many technical possibilities for providing data to patients were showcased at sessions and exhibits. There also were calls by the American Medical Association and others for making such information useful and understandable to patients, who cannot act on information they don’t understand.
- Artificial intelligence (AI) replaced big data. We heard a lot at HIMSS about AI. It has replaced big data – not apparently a dead term – as a HIMSS buzzword, subsumed as a concept under AI, which has evolved as an umbrella term having multiple meanings to many people. For example, people talk about good, old-fashioned decision support but are coating it with an AI overlay. It seems like something new but is still clinical decision support (albeit more precise) at the end of the day.
To be sure, AI and machine learning are rapidly becoming tools to analyze the data needed for patient-specific clinical decision support and value-based care. Despite the hype, there was a bit of a reality check at HIMSS. Now that these tools are becoming available, stakeholders are becoming keenly aware of the sheer volume and complexity of information and the need to deploy it without burdening the physician with an avalanche of data.
- APIs took center stage. The new regulations from ONC and CMS have turned 2019 into the year of the API. Through regulations, standards and technology, there is the expectation that a (free!) API ecosystem will be created for health care. There was a lot of hype at HIMSS about that and the problems it could potentially solve. That said, APIs are not the end all and be all. There are still many details to be thrashed out to make them available and useful including how vendors will recoup their costs while not placing themselves at risk for information blocking. While an API is a recipe for ways to interact, developers still must go through a certification process before their apps can be connected to an electronic health record (EHR). Still to be determined is how developers of certified health IT will “recover costs reasonably incurred” with implementing APIs.
- A focus on the practical. Aside from the hype surrounding APIs and AI, practicality was the focus of many sessions and exhibits. Problem solving is the name of the game. We saw that with the Health Level 7 (HL7) Da Vinci Project’s emphasis on use cases that solve real business problems. Other sessions, such as Humana’s “Payer Insights to the Provider at the Point of Care,” focused on blocking and tackling opportunities to use health IT to deliver data through EHRs to mitigate provider frustrations and make clinical data actionable.
- Fast Healthcare Interoperability Resources (FHIR). FHIR was everywhere at HIMSS. It’s required under the ONC and CMS regulations mentioned previously. The ONC rule looks to promote the adoption of APIs using FHIR, while the CMS rule will hold qualified health plans accountable for using FHIR-based APIs to give Medicare beneficiaries access to their claims data. FHIR also was the basis of many innovations in the exhibit hall and “Interoperability Showcase.” A couple of other announcements slipped under the radar. The first is the set of 15 FHIR resources that health IT modules must support for ONC certification. These are known as the API Resource Collection in Health (ARCH). CMS’ Verma also announced a FHIR-based bulk data access draft specification project but didn’t offer details. The project is aimed at making it easier for accountable care organizations to retrieve Medicare Parts A, B, and D claims data for their beneficiaries.It’s clear that FHIR isn’t a flash in the pan and the obvious government backing of the standard will further drive its accelerated adoption. As a result, stakeholders will need to scale their FHIR knowledge and expertise quickly to meet surge in demand. This also means that other standards development organizations (SDOs) will have to collaborate with HL7, FHIR’s parent SDO, to align standards as use cases evolve for various kinds of health data exchange.
-
 Da Vinci made its mark. The Da Vinci Project for which POCP is the project management organization, really had a big showing at HIMSS. This new private-sector initiative is developing a rapid multistakeholder process using FHIR to address value-based care data exchange use cases between payers and providers. Da Vinci’s use cases address real business problems and interoperability, as highlighted in demonstrations at the Interoperability Showcase. Different payers were rotated through to show how transactions can flow successfully among different stakeholders. Da Vinci also was highlighted by payers, providers, and ONC and CMS representatives at various sessions, including sessions moderated by POCP’s Jocelyn Keegan, Da Vinci project manager.
Da Vinci made its mark. The Da Vinci Project for which POCP is the project management organization, really had a big showing at HIMSS. This new private-sector initiative is developing a rapid multistakeholder process using FHIR to address value-based care data exchange use cases between payers and providers. Da Vinci’s use cases address real business problems and interoperability, as highlighted in demonstrations at the Interoperability Showcase. Different payers were rotated through to show how transactions can flow successfully among different stakeholders. Da Vinci also was highlighted by payers, providers, and ONC and CMS representatives at various sessions, including sessions moderated by POCP’s Jocelyn Keegan, Da Vinci project manager.
However, Da Vinci’s momentum is best exemplified by being singled out by name in the proposed CMS rule including specific mention of Da Vinci’s Coverage Requirements and Documentation Rules Discovery use case and a direct statement that encourages all payers to align with the Da Vinci Project “to build an ecosystem that will allow providers to connect their EHRs or practice management systems and efficient work flows with up-to-date information on which items and services require prior authorization and what the documentation requirements are for various items and services under that patient’s current plan enrollment.”
- There were few new EHR vendors. Normally, HIMSS is a place for new EHR vendors to strut their stuff. The cheap seats on the fringes of the exhibit halls are usually chock full of new entrants into the EHR market. Not so much this year. We wonder if this is indicative of the consolidation that has occurred in that market, the expense of attending HIMSS or both. We also wonder if it’s because the grab for EHR customers is over, so vendors are focusing on how to optimize revenue and provide more value to users.
That said, we saw some vendors focused on the long-term and postacute care market. These sites of care have their own specific health IT needs and challenges. Addressing them is an emerging area that we can expect to see more about as 2019 rolls on.
The POCP team was actively engaged at HIMSS and it was our best year yet. What we have reported here is a drop in the bucket. Want to know more? Reach out to me at tonys@pocp.com.


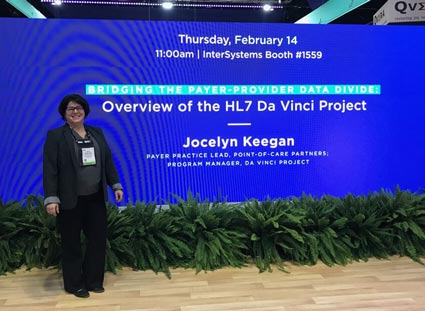 Da Vinci made its mark. The Da Vinci Project for which POCP is the project management organization, really had a big showing at HIMSS. This new private-sector initiative is developing a rapid multistakeholder process using FHIR to address value-based care data exchange use cases between payers and providers. Da Vinci’s use cases address real business problems and interoperability, as highlighted in demonstrations at the Interoperability Showcase. Different payers were rotated through to show how transactions can flow successfully among different stakeholders. Da Vinci also was highlighted by payers, providers, and ONC and CMS representatives at various sessions, including sessions moderated by POCP’s
Da Vinci made its mark. The Da Vinci Project for which POCP is the project management organization, really had a big showing at HIMSS. This new private-sector initiative is developing a rapid multistakeholder process using FHIR to address value-based care data exchange use cases between payers and providers. Da Vinci’s use cases address real business problems and interoperability, as highlighted in demonstrations at the Interoperability Showcase. Different payers were rotated through to show how transactions can flow successfully among different stakeholders. Da Vinci also was highlighted by payers, providers, and ONC and CMS representatives at various sessions, including sessions moderated by POCP’s 